How and when to authorize planned services
How to determine when an authorization is required
As authorization requirements can vary by Member benefit plan and type of service, it is always important to verify when a preauthorization is required before those services are provided.
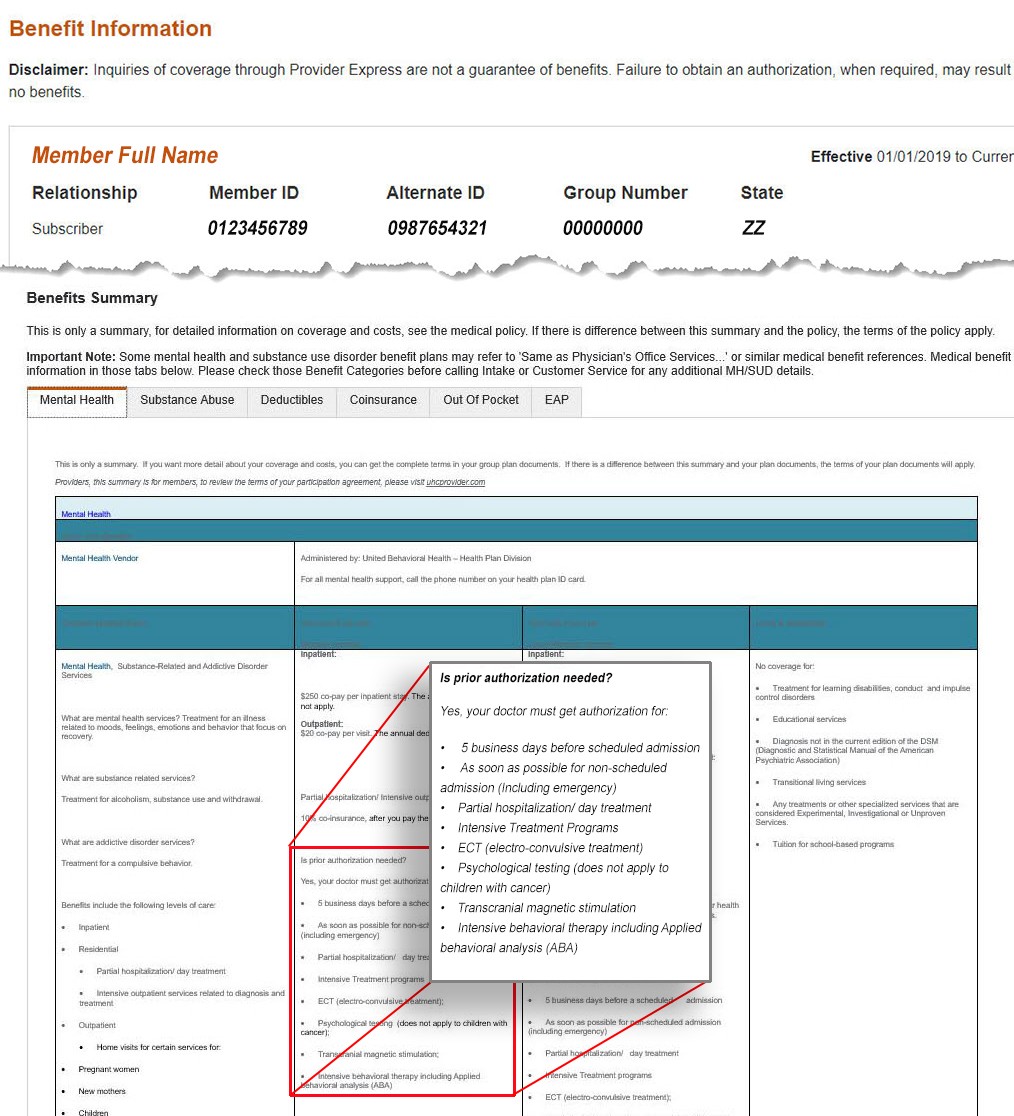
We make it easy to verify what services need an authorization through our online tools on Provider Express. Start by looking up the Member’s eligibility and benefits to see what services require an authorization. (Hint: check out our video on Member Eligibility & Benefits for step-by-step instructions). In the example screenshot included below, you can see an authorization is required for inpatient services for this member.
Non-routine services do require an authorization
- These can be requested online for select services
- Frequently used non-routine services where an authorization can be requested online include:
- Psychological Testing - Click here for online request form
- Transcranial Magnetic Stimulation (TMS)
- ABA/Autism - To determine the authorization required Click here to be directed to the ABA page
For all other non-routine services please call the number on the back of the Member's ID card to request authorization.
- Claims submitted for services which require authorization, where no prior authorization is found, will be denied.